
Fall Deaths More than Double for Seniors Age 65+
Roughly one in four people age 65+ report an accidental fall each year.1 For some seniors, these accidents can be deadly. Falls are the number one cause of accidental injury deaths among seniors.2 What’s more, a recent CDC bulletin reports that fall deaths and the fall-death rate have risen steadily since the turn of the century. We’ve seen more than a 250% increase in the number of fall deaths, rising from 11,722 in year 2000 to 29,668 in 2016.3,4
Fall Death Rate More Important than Number of Fall Deaths
Of course, one can attribute part of that increase to changing demographics. The number of seniors in our population is growing. However, there is more to it. The rate of fall deaths among seniors is on the rise as well. That can’t be explained away by demographics – not entirely at least. From 2007 to 2016, the rate of fall deaths among seniors grew 31%.4
Number of deaths from falls and age-adjusted rates among adults aged ≥65 years — United States, 2007–2016
Source: Burns E, Kakara R. Deaths from Falls Among Persons Aged ≥65 Years — United States, 2007–2016. MMWR Morb Mortal Wkly Rep 2018;67:509–514.
Fall Death Rates Vary by State
Interestingly, this data may not apply to you. In the most recent analysis, fall death rates increased in 30 states and Washington DC. The 10-year rate actually declined in Vermont, New Mexico, and Hawaii. That doesn’t mean these states are safer than the rest, unfortunately. Vermont and New Mexico rank among the top ten states with the highest fall rates along with Wisconsin, Minnesota, Colorado, South Dakota, Oregon, Rhode Island, Oklahoma, and New Hampshire.
The ten states with the lowest fall death rates are:
- Alabama
- New Jersey
- Delaware
- Louisiana
- California
- New York
- Indiana
- Arkansas
- Kentucky
- Hawaii
Death Rate from Falls, 2016 (Number of Deaths per 100,000 people age 65+)
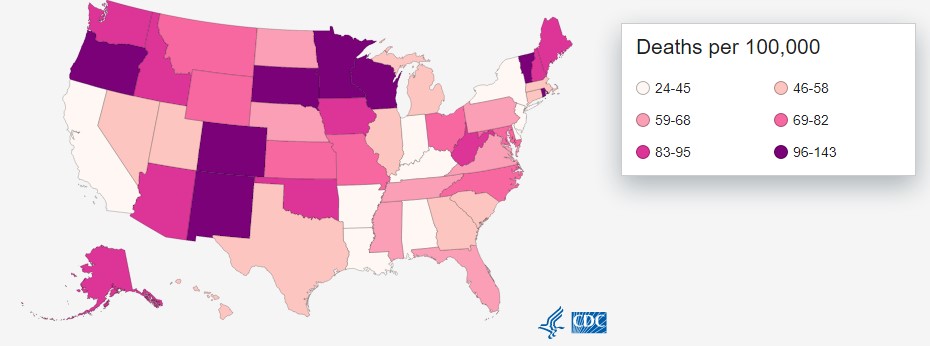
Source: CDC
Why is the Fall-Death Rate Increasing?
The aging population explains only part of the increase. People age 85+ prove more likely to fall than people age 65 to 84, and people age 85+ are a growing portion of the senior population. Also, the 31% increase is measured after adjusting fall rates for age. Therefore, the changing demographics do not fully explain the increasing rate of fall deaths.
Increasing rates of polypharmacy (having 5 or more meds) may play a role. The most likely explanation is that survival after the onset of common diseases such as heart disease, cancer, and stroke is on the rise.5 Naturally, as death rates from top diseases fall, something else must take their places.
Taking a Stand Against Falls
The good news about the rise of fall deaths is that many accidental falls are preventable. Doctors should be screening for fall risk in annual senior wellness exams.4 Among seniors with a high risk of falls, fall prevention programs that target multiple risk factors have been shown to reduce the rate of falls.6 Home health stands out as a primary source for fall injury prevention programs. When seniors qualify, Medicare pays 100%. Home health sends nurses and therapists to the homes of seniors for medication review, home safety assessment, gait training, fall safety training, and more.
References:
- National Center for Health Statistics. Health, United States, 2016: with chartbook on long-term trends in health. Hyattsville, MD: US Department of Health and Human Services, CDC, National Center for Health Statistics; 2017.
- Bergen G, Stevens MR, Burns ER. Falls and fall injuries among adults aged≥ 65 years—United States, 2014. Morbidity and Mortality Weekly Report. 2016 Sep 23;65(37):993-8.
- Hu G, Baker SP. Recent increases in fatal and non-fatal injury among people aged 65 years and over in the USA. Injury Prevention. 2010 Feb 1;16(1):26-30.






